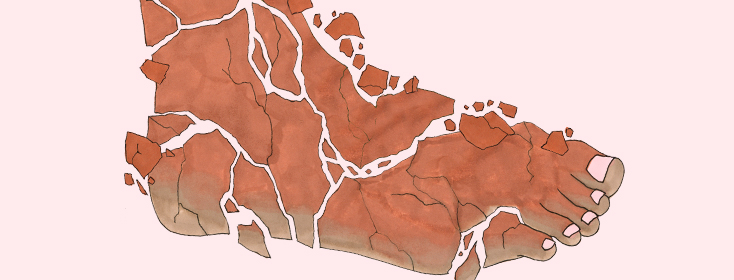
The Psoriatic Foot
Significant pain when walking? Scaly plaques on the soles of the feet? Deep cracks and bleeding on the foot or both feet?
How do psoriasis and psoriatic arthritis affect the feet?
These could be signs that you might be experiencing symptoms of psoriasis on your feet, or palmoplantar psoriasis (PP) a condition in which psoriasis impacts the soles of the foot or feet. It could also be a sign of palmoplantar pustular psoriasis (PPP), which is a variant of psoriasis that can limit the ability to walk, work and perform routine daily activities.
What symptoms occur with PP and PPP?
Symptoms of palmoplantar psoriasis (PP) include pustules, nail involvement, painful fissures (cracking), and thick, scaly, plaques typically on the soles of the feet.
Symptoms of palmoplantar pustulosis also include sterile intraepidermal (occurring between the layers of the skin) pustules, erythema (redness), fissuring (cracking), and scaling. PPP has a strong association with smoking and occurs more frequently in women.
While the inflammatory pathways that are involved in palmoplantar pustular psoriasis have not been studied as well as those of plaque psoriasis, there has been research that demonstrates there are increased levels of cytokines, including IL-17 and IL-22 with PPP. Cytokines have a variety of functions, but most are involved in directing other immune cells to perform a certain behavior. Studying these interleukins may help to pinpoint how treatments will impact the immune system response.2
Psoriatic arthritis in the foot
Psoriasis on the feet can also become more challenging if you also are diagnosed with psoriatic arthritis. Psoriatic arthritis can affect the feet in several ways. The joints in the toes can become inflamed and may cause sausage-like swelling of the toe. In addition, some people with psoriatic arthritis experience pain at the arch of the foot or in the heel, this pain is caused by inflammation at the attachment points of the tendons and ligaments. Pitting, thickening and lifting of the nail from the nail bed are also signs of psoriatic arthritis of the foot.
Treatment depends on the severity of the disease
PP is usually managed with topical therapy as a first step. Systemic therapy is needed when the topicals fail or the disease becomes more severe. Psoriasis on the feet can impair the ability to work or to do daily activities and can have a huge impact on the patients’ quality of life, so it is important to discuss treatment options with a medical provider.
For mild cases of psoriasis, there are some topical options that may be suggested by a provider. Coal tar products are an option, coal tar products can come in cream, gel or ointment forms. Coal tar can help with slowing the growth of skin cells and reducing plaques, it also can help with the inflammation and itchiness. Salicylic acid may be used as a product that can be used to soften or remove thickened scales. Your healthcare provider may recommend topical corticosteroids, which are applied directly to the impacted area. Phototherapy may also be an option for treatment. Combinations of certain therapies may also be suggested as they often work better than one treatment alone.
Best foot forward
Wet wrap therapy can also be an option. Wet wrap therapy involves bathing then covering the area with a topical corticosteroid ointment, then covering it with wet clothes (or some use saran wrap.) Some leave the wet wrap on overnight, or for a couple hours. This process helps moisturize the skin and allows the medicine to penetrate the skin.
For moderate to severe cases these may require systemic (whole body) treatments. Certain biologic drugs may also be an option for severe cases or if other treatments have not made an impact.
What things have you tried that have helped manage your psoriatic feet?
Join the conversation